

Summer and fall of 2021 will bring new challenges to the U.S., as the nation enters a new phase of the COVID-19 pandemic. Falling infection rates and deaths, due largely to vaccinations, are bringing relief and hope to large swaths of the country, and employers, schools, and others are looking forward to a return to normal operations. However, for the immense number of people who have been directly impacted by COVID-19, this return to normal may be difficult to achieve, as significant stress, trauma, and grief continues. For health care workers, in particular, the unique challenges of COVID-19 continue to impact mental health and well-being.
Throughout the pandemic, health care workers encountered innumerable challenges, including developing and implementing new safety protocols, often with limited PPE or other resources; working long and difficult hours, sometimes away from home in harder-hit areas in need of help; encountering emotional and ethically challenging decisions about scarce resource allocations; and, especially, facing the loss of patients to the disease, and working with families grieving their losses. Exhaustion, fear of exposure and illness, grief, and isolation have significantly impacted health care workers during this time.
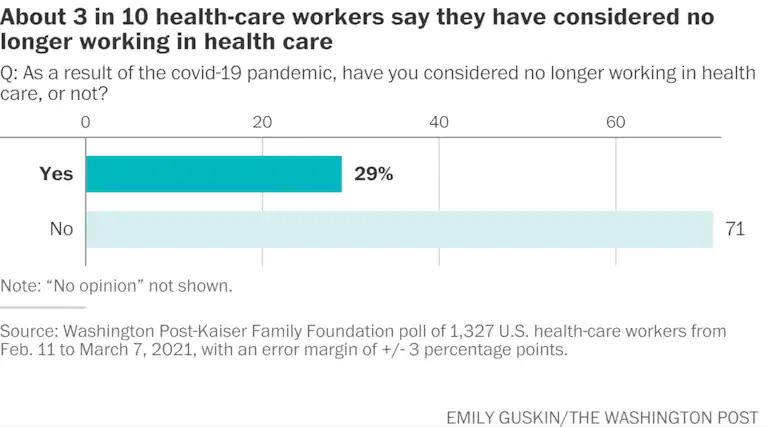
In April 2021, a UNC Health psychiatrist reported that the number of health care workers seeking mental health care had increased 400% from pre-pandemic levels. A Washington Post-Kaiser Family Foundation poll found that about 6 in 10 health care workers said stress from the pandemic has affected their mental health, and approximately 3 in 10 health care workers have considered leaving their profession.
In this poll, 6 in 10 health care workers expressed frustration with people not taking enough precautions to prevent the spread of COVID-19; while these workers felt that most people appreciated their work caring for COVID-19 patients, many felt disrespected and endangered by individuals’ decisions to inadequately follow public health guidance to slow infections.
Even prior to the pandemic, several NCIOM task forces and state experts had identified health care workforce development as a key issue for our state. Shortages in nursing; inadequate access to primary and specialty care, especially in rural areas; and the need for training and wage support for frontline health care workers such as certified nursing assistants and home health aides all require action and investment to ensure that North Carolinians have the care they need. As policymakers, educators, and health systems determine appropriate and effective investments in our health care workforce, it is crucial to also prioritize the mental health support workers need as they recover from the impacts of the pandemic – and care for those who cared for us when we needed it most.