

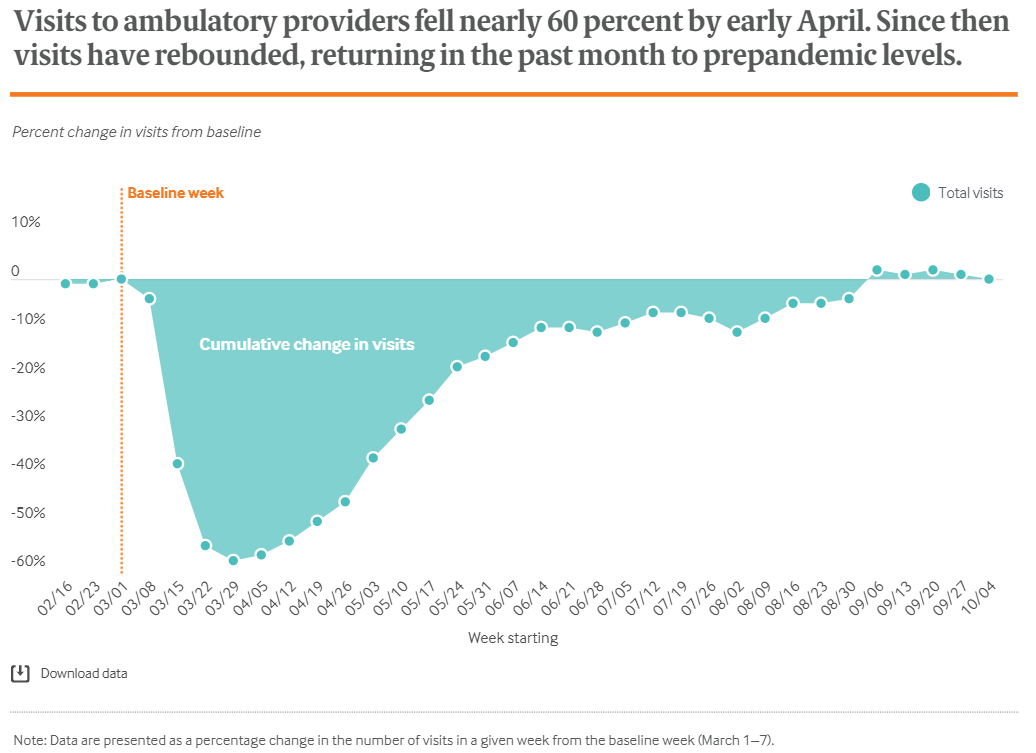
In the early weeks and months of the pandemic, there was a dramatic decline in the utilization of health care for emergent needs, elective procedures, and preventive care, such as well visits and vaccinations. Outpatient care declined by nearly 60 percent by late March, but after restrictions on nonessential travel were lifted in most states, overall visits to ambulatory providers returned to their baseline levels.
However, the visits for specific age groups and preventive care remain well below pre-pandemic levels. In late March, wellness visits and vaccination rates fell precipitously for children aged 0-2, an age when most childhood vaccinations are administered. As of October, visits for children aged 0-2 are still 18% below the baseline. The CDC issued guidance emphasizing the importance of routine child care and immunizations, and research from the CDC warns that this foregone care may result in outbreaks of vaccine-preventable diseases. Between March and June, an estimated 285,000 breast cancer, 95,000 colon cancer, and 40,000 cervical cancer screenings were missed.
While the potential long-term clinical impacts of this foregone care have yet to be seen, the trend has caused immediate financial impacts to providers and health care systems.
The American Hospital Associated estimated a total of $202.6 billion in lost revenue between March 1 and June 30 for hospitals and health systems. Hospitalizations for non-COVID care continue to remain low, and smaller and rural hospitals are the most likely to face financial challenges due to COVID-19. Rural hospitals in North Carolina, which often operate on razor-thin margins, have canceled or delayed elective procedures that are a key source of revenue. Independent primary care practices have experienced significant financial loss, and one study estimated the average primary care practice would lose $57,190 per full-time physician, while rural non-Federally Qualified Health Centers were projected to lose $75,274 per full-time physician. In June, BlueCross BlueShield of North Carolina announced the Accelerate to Value program to provide financial support through lump payments in 2020 and 2021 to providers willing to remain independent and join an accountable care organization.
NCIOM’s 2020 Annual Meeting will take place virtually and will further explore the impact of foregone care during the pandemic, including long-term impacts on population health and the health system. Panelists and speakers will discuss the factors that drive these impacts, such as changes in insurance coverage, capacity of the health system, changes to models of care and payment models, and drivers of health.