

Written by Emily Hooks
As COVID-19 cases increase throughout our state and nation, social distancing guidelines have caused Americans to restructure most of our daily routines. To adhere to social distancing guidelines and shelter-in-place orders, people are largely dependent on internet service through their computers, tablets, or smart phones to connect them with their work, education, and health services. Those who do not have access to adequate internet coverage or other technological resources experience the “digital divide,” which has disparate impacts for low-income and rural Americans.
The most immediate impact of the digital divide during this pandemic is a lack of access to telehealth. Telehealth encompasses both clinical services provided remotely through telecommunication technologies and additional health services provided through these means, such as staff training, administrative services, and public health activities. According to HRSA, these technologies include video conferencing, the internet, store-and-forward imaging (sending clinical data electronically to another site for evaluation), streaming media, and terrestrial and wireless communications. The CDC has encouraged health care facilities and providers to utilize telehealth to reduce transmission of coronavirus, in part by reducing the number of patients in waiting rooms.
Last Tuesday, the Trump administration announced expanded Medicare coverage for telehealth clinical visits so older Americans could access health care services from home and reduce the risk of exposure to COVID-19 for both patients and health care providers. Prior to this announcement, Medicare coverage for telehealth was more narrow and only paid clinicians for routine visits for patients living in rural areas. Telehealth services will be paid for at the same amount as in-person services. Private payers are also increasing their coverage of telehealth services; in North Carolina, the largest private insurer, Blue Cross and Blue Shield of North Carolina, has issued a new policy covering telehealth services at the same payment rate as in-person visits. Blue Cross and Blue Shield is also eliminating cost-sharing for telehealth services and including audio visits in these policies. In addition, North Carolina Medicaid is requesting a temporary waiver from the federal Centers for Medicare and Medicaid Services to increase flexibility around enhanced telehealth services during the COVID-19 pandemic.
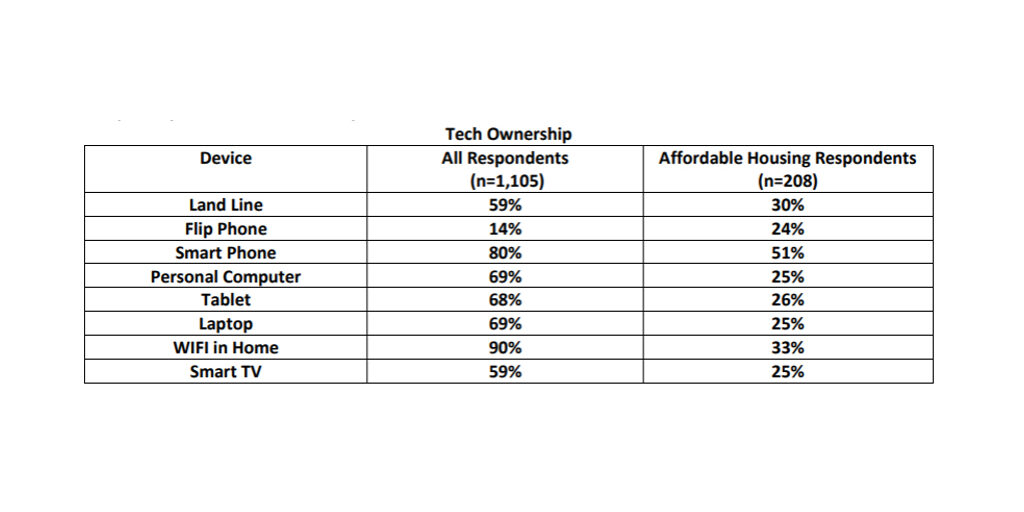
Telehealth is an important method for individuals, especially older adults who are at higher risk of severe illness and death from COVID-19, to avoid contact with those who have the virus. Telehealth also allows for improved access and quality of care for low-income and rural patients who will still need health services for other illnesses or chronic conditions. However, the ability to access telehealth services relies on the individual having access to a computer, tablet, or smart phone and internet or 3G cell service. In a 2019 study of individuals 55 and older, there was a large discrepancy between affordable housing respondents’ ownership of technologically capable devices and the overall demographic of older adults.
Several North Carolina Institute of Medicine task forces and stakeholder groups have identified improved broadband access and reduction of the digital divide as a crucial step to improve access to health care and increase health equity. Most recently, the Task Force on Serious Illness Care recommended continued robust investment in broadband access throughout the state in order to improve access to telehealth services and communication between health care providers.
In light of the COVID-19 pandemic, the digital divide and the actions needed to address it are coming into stark relief. NCIOM stakeholders have identified action from public and private health care payers to increase payment for telehealth services, combined with policies to improve the technological infrastructure necessary for these services, as critical to meet the state’s needs.